Winter brings more than a chilly breeze; it comes with pesky coughs, runny noses, sore throats, congestion, colds, or even the flu. Using the right medications can help alleviate symptoms ranging from muscle aches to fevers and headaches, whether prescription or Over-the-Counter (OTC). When breastfeeding, there is an extra person to worry about when choosing medicine. A major factor to keep baby healthy is by taking care of mom. We want our breastfeeding mothers equipped with the proper knowledge to combat any ailments they could face--while keeping baby safe.
Looking for a quick list of safe medications while breastfeeding? Try our 1-page flyer.
In This Article
Combination Product Overview
Prescription Antibiotics & Steroids
Herbal & Nutritional Supplements
Looking for information on other meds?
Lactation Risk Categories Explained
This article uses Dr. Hale’s Lactation Risk Categories. Each medication is assigned a rating from Safest (L1) to Hazardous (L5).You can find more information on this rating system at the bottom of this page.
Combination Product Overview
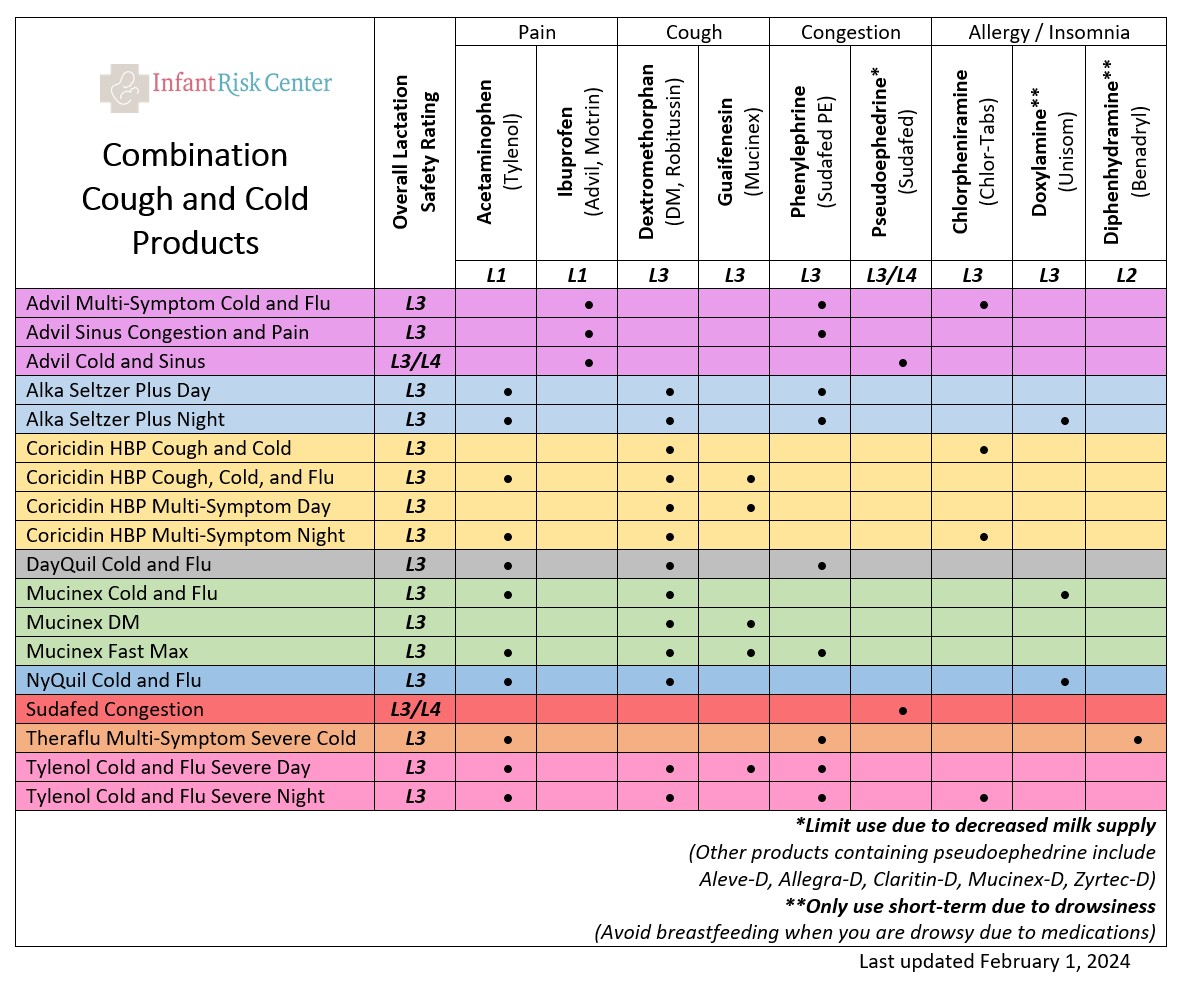
Everyone loves a good combination product with everything you need for a cough or cold. But there are so many options...what is in them, and what is compatible with breastfeeding? The chart below will help you break it down. Then, you can read about specific drugs below!
What can I take for Pain & Fever while Breastfeeding? (analgesics and antipyretics)
Ibuprofen (L1): The transfer of ibuprofen in breast milk is well studied as it is a common choice for postpartum pain. Very little of this medication makes it into the milk (about 0.6% of the mother’s dose). In addition, this drug is given directly to babies at much higher doses than this.2 Ibuprofen is the preferred analgesic in breastfeeding mothers. Do not exceed 3.2 grams/day. Common Trade Names: Advil, Nuprin, Motrin.
Acetaminophen (L1): Acetaminophen is compatible with breastfeeding as only small amounts are secreted into breast milk. This is given directly to infants in doses much greater than they would receive incidentally through the breastmilk. Acetaminophen is commonly included in combination products. Do not exceed 4 grams/day. Common Trade Name: Tylenol.
Naproxen (L3): Naproxen is less well studied than the other drugs in the same class. It is secreted into the breastmilk, but apparently not in quantities that would harm an infant. However, naproxen takes longer to be eliminated from the body than the other NSAIDs and has a greater potential to damage an infant’s cardiovascular system, kidneys, and gastrointestinal tract in the event of an overdose. Short-term use (<2 weeks) of naproxen postpartum, or infrequent or occasional use should be compatible with breastfeeding. Do not exceed 1 gram/day. Common trade names: Naprox, Naprosyn, Aleve.
Aspirin (L2): Although aspirin is secreted into breast milk in small quantities, it has the potential to cause bleeding problems in infants and increases the risk of Reye syndrome (liver damage associated with using aspirin to treat certain viral illnesses in children). The use of “baby aspirin (81 mg per day)” is unlikely to increase the risk of these problems. Aspirin should not be the first choice for pain relief in breastfeeding mothers. However, the benefits of its unique pharmacology may outweigh the risks for women with certain conditions like rheumatic fever and after heart attacks. The decision to use aspirin should be undertaken with physician guidance. Common trade name: Bayer.
*Some combination headache or menstrual relief medicines that contain aspirin or acetaminophen, like Excedrin or Midol, contain caffeine. See our discussion on caffeine for more information.
What can I take for Cough & Chest Congestion while Breastfeeding?
Benzocaine (L2): Numbing Agent. Temporarily relieves pain associated with itching, sore throat. There are no adequate and well-controlled studies or case reports in breastfeeding women. Due to its low oral absorption after application, maternal blood concentrations are probably too low to produce any significant clinical effects in the breastfed infant. Benzocaine cough drops or lozenges (with or without menthol) are an excellent choice for cough relief in breastfeeding mothers. Common trade names: Cepacol.
Menthol (L3): Numbing Agent. Commonly used for topical analgesics and sore throat relief. Only minimal amounts of Menthol would be transferred into breast milk. Adverse effects to infants from breastfeeding are unlikely due to low relative dose and first-pass metabolism. There are no adequate and well controlled studies in breastfeeding women. Menthol cough drops, lozenges, and/or chest rub are an excellent choice for cough relief in breastfeeding mothers. Common trade names: Halls, Ricola, Luden’s, Vick’s
Guaifenesin (L2): This is an expectorant used to loosen respiratory tract secretions. It does not suppress coughing. The poor efficacy of expectorants in general would suggest that they do not provide enough justification for use in breastfeeding mothers. However, untoward effects to the infants have not been described. Common trade names: Robitussin, Mucinex
Honey (L3). According to a study in 2014, honey was more efficacious in treating cough symptoms in children than placebo and diphenhydramine, but was less efficacious than dextromethorphan.3 Further studies need to be considered in adults, however. Honey should never be consumed by infants.
Dextromethorphan (L3): This is an antitussive drug that appears to work by elevating the cough threshold in the brain. It is the safest of the antitussives and unlikely to transfer into milk. Watch breastfed infants for drowsiness or poor feeding. Common trade names: DM, Benylin, Delsym, Robitussin DM.
Benzonatate prescription required (Avoid when possible, L4): Non-narcotic cough suppressant. There are minimal pharmacokinetic data on this product, and no data on transfer to human milk. Milk transfer is expected to be low-moderate based on the medication size. Benzonatate is a very dangerous product when taken directly by a child. Due to this potential for severe toxicity at relatively low doses, this medication should be avoided in lactation. Common trade names: Tesselon Perles
Codeine prescription required (L3): Although no longer available over the counter, drugs containing codeine are used to treat pain and cough. Codeine can cause respiratory depression when taken in high doses. While there have been scattered cases of respiratory depression in breastfeeding infants, it is likely safe to consume in moderate amounts (<150 mg per day) while breastfeeding. In general, if the mother is lethargic she should wait to breastfeed until she is alert, at which point codeine levels would be lower. Common trade names of combination products: Cheratussin AC, Tuzistra XR, Robitussin AC, Vanacof, Tylenol #3, Tylenol #4
What can I take for Allergies & Sinus Congestion while Breastfeeding?
Diphenhydramine (L2): Antihistamine. Diphenhydramine is an antihistamine that is often used in cough, cold, sinus, and allergy formulations. It is also the main component in many sleep aids, including “nighttime” versions of cold medications, as well as motion sickness pills. Although the levels are low in breastmilk, this medication can cause sedation and therefore is not ideal in breastfeeding mothers. If you are taking a sedating medication, be sure to have support in caring for your infant. There are many non-sedating antihistamines on the market, which are likely a better choice. These include cetirizine (Zyrtec-L2), loratadine (Claritin, Alavert- L1), and fexofenadine (Allegra- L2). There is some anecdotal evidence that diphenhydramine can suppress milk production, but this pattern is not supported by the medical literature. Common trade names: Benadryl, Tylenol PM.
Chlorpheniramine (L3) and Brompheniramine (L3): Antihistamine. These medicines are similar to diphenhydramine, but they have fewer studies about breast milk safety. They are heavily sedating and not recommended. If you are taking a sedating medication, be sure to have support in caring for your infant. The non-sedating antihistamines mentioned above are still better choices. Common trade names: Aller-Chlor, C.P.M., Chlor-Phen, Chlor-Trimeton Allergy, Teldrin HBP.
Pseudoephedrine over-the-counter, but kept in pharmacy (L3): Decongestant. Pseudoephedrine is an adrenergic compound used as a nasal decongestant. It does not have antihistamine properties. It is excreted into breast milk in low levels. Caution should be used with this product as it may reduce milk production in some mothers in late stage lactation (mothers breastfeeding infants >8 months old). Pseudoephedrine commonly appears in combination products. An excellent alternative would be a nasal decongestant like oxymetazoline (Afrin-L3 discussed below).Common trade names: Sudafed, Claritin-D.
Phenylephrine (L3): Decongestant. Phenylephrine is a decongestant that is commonly added to cold mixtures and nasal sprays for use in colds, flu, and congestion. A recent statement was released by the FDA that concluded that oral phenylephrine is NOT effective as a decongestant. An excellent alternative would be a nasal decongestant like oxymetazoline (Afrin-L3 discussed below). Common trade names: Neofrin, Neosynephrine, Vicks Sinex Nasal.
What can I take for Nasal Congestion and Swelling while Breastfeeding? (Nasal sprays)
Nasal Saline Irrigation (L1): Using salt water to irrigate the nose and sinuses is a practice dating back thousands of years. In modern pharmacies, saline is available in nasal sprays and nasal rinses, as well as mineral packets for home reconstitution. Studies have shown sinus and nasal rinsing to be highly effective in relieving symptoms of chronic rhinosinusitis.4 Saline irrigation is the safest possible treatment for rhinosinusitis in pregnant or breastfeeding mothers. A randomized controlled trial in 2024 presented at the European Respiratory Society Congress found that using hypertonic saline nasal drops shortened cold symptoms in children by two days (6 days vs. 8 days with usual care) and reduced medication use. The study of 301 infected children also showed fewer household members caught colds when saline drops were used (46% vs. 61%). Researchers suggested that chloride in the salt helps suppress viral replication, improving recovery and reducing transmission. Common Trade names: Sinus Rinse, Simply Saline, Ocean.
Oxymetazoline (L3): Nasal Decongestant. This decongestant comes in several formulations that last between 4 and 12 hours. There are no good studies of oxymetazoline safety during breastfeeding, however, very little of it is expected to reach the milk because it is locally administered and poorly absorbed. For this reason, oxymetazoline is probably a better choice than oral systemic decongestants such as pseudoephedrine during breastfeeding. Oxymetazoline should only be used briefly, no more than 3 days, to avoid rebound congestion. Common trade name: Afrin.
Triamcinolone (L3): Nasal Steroid. This is the first OTC steroid nasal spray to be marketed in the United States. Triamcinolone may be used for longer periods of time without causing rebound congestion. There is virtually no risk to a breastfeeding infant when the mother uses this product nasally. Oral and topical forms (by prescription only) deserve more caution in their use. Common trade name: Kenalog shot, Nasacort.1
Fluticasone (L3): Nasal Steroid. A typical steroid primarily used intranasally for allergic rhinitis and via inhalation for asthma. With limited oral and systemic bioavailability, it is not likely that milk levels will be clinically relevant, even with rather high doses. No effects have been reported in breastfeeding infants. Common Trade names: Flonase.
Mometasone (L3): Nasal Steroid. Primarily intended for intranasal and topical use. It is considered a medium-potency steroid. It is extremely unlikely mometasone would be excreted in human milk in clinically relevant levels following topical or intranasal administration.There were no reported health concerns via milk.Common Trade names: Nasonex.
What can I take to help with Sleep while Breastfeeding?
Diphenhydramine (L2): Antihistamine. Diphenhydramine is an antihistamine that is often used in cough, cold, sinus, and allergy formulations. It is used to dry up secretions. Sedation is an unwanted side effect when using it as an allergy medication, but can be an advantage to help with sleep. If you are taking a sedating medication, be sure to have support in caring for your infant. There is some anecdotal evidence that diphenhydramine can suppress milk production, but this pattern is not supported by the medical literature. Common trade names: Benadryl, Tylenol PM.
Doxylamine (L3): This is another sedating antihistamine, similar to diphenhydramine, which is more commonly used for its sedative properties. There are no good studies about how much of this drug gets into breast milk. In infants exposed to doxylamine, there are reports of sedation, apnea, and paradoxical CNS stimulation. If you are taking a sedating medication like diphenhydramine, be sure to have support in caring for your infant. Use caution with this medication. Common trade name: Unisom
Melatonin (L3): Melatonin is a normal hormone secreted by the pineal gland in the human brain, mostly at night. It may either induce a sleep-like pattern in humans, or be the result of sleep; the evidence is not clear. It is definitely passed into human milk and some experts believe it is responsible for entraining the newborn brain to reset its circadian clock to that of the mother by communicating the time of day to the newborn. The effect of orally administered melatonin on newborns is unknown, but no adverse reactions have been reported so far.
Are Prescription Antibiotics & Steroids Safe while Breastfeeding?
Antibiotics prescription only (typically L1-L2): In general, it is safe to breastfeed while on a short course (<14 days of antibiotics). These medications typically transfer into milk in acceptable amounts. Some infants can be sensitive to even small amounts in their GI tract, causing diarrhea. If age appropriate, probiotics or yogurt with live cultures can be used to minimize GI upset (for you too mom!). Common names: penicillins, cephalosporins, azithromycin
Steroids prescription only (typically L2): Short term courses of oral or injectable steroids are unlikely to affect breastfed infants. Doses used for respiratory infections do not require any interruption to breastfeeding. Common names: methylprednisolone (Medrol dose pack, SoluMedrol), prednison, prednisolone, budesonide (Pulmicort), triamcinolone (Kenalog)
What Herbal & Nutritional Supplements can I take for a cold while Breastfeeding?
Zinc nutritional supplement (L2). Zinc can be used topically or ingested, and is usually not harmful when breastfeeding an older infant. However, doses of zinc in cold remedies can be in excess of what is safe. There is no accepted standard for what is too much, but the recommended daily allowance of zinc from all sources (including food) is 12 mg per day in a lactating woman. Doses of commonly marketed zinc supplements frequently range from 8-25 mg taken every 3-4 hours. Total daily zinc consumption can become easily excessive with these products. Zinc salts for cold treatment can have possible negative effects on breastfeeding infants during the first weeks of life. Thus, excessive zinc supplementation in breastfeeding mothers should be avoided for the first month postpartum. Topical application of zinc oxide (like sunscreen) is not absorbed, and is safe when breastfeeding. Common trade names: Galzin, Airborne, Orazinc, Zicam
Vitamin C nutritional supplement (L1). Vitamin C is often advertised for cold-fighting. Although its efficacy in treating colds has not been supported, it likely is not harmful to supplement while breastfeeding. Even high levels of maternal consumption resulted in only slightly increased levels in breastmilk.5 Common trade names: Emergen-C, Cenolate, Celin, Cemill (double check ingredients to make sure zinc concerntrations are
Echinacea herbal supplement (L3). is an herb that has been shown to have significant antitussive effects when taken as an oral supplement.6 Although it is likely safe to take while breastfeeding, there have been no significant studies showing the effects of Echinacea consumption on breastfeeding infants or milk production.
Elderberry herbal supplement (L3). is a herb used to shorten the duration of cold and flu symptoms. Although it is likely safe to take while breastfeeding, there have been no significant studies showing the effects of Elderberry consumption on breastfeeding infants or milk production.
Propolis herbal supplement (L2). is a resin produced by bees that is commonly used for sore throats and cold symptoms in the form of a throat spray. It is likely safe when used orally during lactation. Propolis 300 mg daily was used for 4-10 months in one clinical study with no adverse effects breastfed infants.
Oscillococcinum homeopathic supplement (L3). is used to treat cold and flu symptoms, however, studies have shown that it this supplement is unlikely to be helpful. There have been no significant studies showing the effects of Oscillococcinum consumption on breastfeeding infants or milk production.
Looking for information on other meds?
The MommyMeds app provides up-to-date knowledge on various medications for the safe use of breastfeeding mothers. Our diverse team of specialists have come together to develop an easy to use resource accessible to mothers regarding drug related lactation risk. Support our research on breastfeeding medication by downloading the app today.
(For other ailments, see our sections on acne and GI complaints.)
Lactation Risk Categories Explained
Drs. Thomas Hale and Kaytlin Krutsch have performed extensive research on the effects of medications in mother’s milk. They have given each medication a rating from Safest (L1) to Hazardous (L5).
L1 Safest: Extensive evidence demonstrating no adverse effects on the infant
L2 Safer: Limited evidence without an increase in adverse effects on the infant
L3 Probably Safe: No studies, but expert opinion suggesting safety. Risk to the infant is possible, and further evaluation must be taken to consider individual situations.
L4 Possibly Hazardous: Positive evidence or expert opinion of risk to the infant or milk production.
L5 Hazardous: Significant and documented risk to the infant.
Kaytlin Krutsch, PharmD, MBA, BCPS
Nichole Campbell, MSN, APRN, NP-C
Emily Conard, PharmD, MBA
Last updated on 1/9/2025
Adapted from previous InfantRisk articles authored by James Abbey, MD, Thomas W. Hale, Ph.D., and Teresa Baker, MD.
References
1. Hale, Thomas Wright. Hale's Medications & Mothers' Milk, 2021: A Manual of Lactational Pharmacology. Springer Publishing Company, 2021.
2. Walsh P, Rothenberg SJ, Bang H. Safety of ibuprofen in infants younger than six months: A retrospective cohort study. Leong C, ed. PLOS ONE. 2018;13(6):e0199493. doi:10.1371/journal.pone.0199493
3.Findlay, Jw, et al. “Pseudoephedrine and Triprolidine in Plasma and Breast Milk of Nursing Mothers.” British Journal of Clinical Pharmacology, vol. 18, no. 6, 1984, pp. 901–906., doi:10.1111/j.1365-2125.1984.tb02562.x.
4. Achilles N, Mosges R. Nasal saline irrigations for the symptoms of acute and chronic rhinosinusitis. Current allergy and asthma reports. Apr 2013;13(2):229-235.
5. Fung EB, Ritchie LD, Woodhouse LR, Roehl R, King JC. Zinc absorption in women during pregnancy and lactation: a longitudinal study. Am J Clin Nutr 1997; 66(1):80-88.
6. Barth, Anders, et al. “Antitussive Effect of a Fixed Combination of Justicia Adhatoda, Echinacea Purpurea and Eleutherococcus Senticosus Extracts in Patients with Acute Upper Respiratory Tract Infection: A Comparative, Randomized, Double-Blind, Placebo-Controlled Study.” Phytomedicine, vol. 22, no. 13, 2015, pp. 1195–1200., doi:10.1016/j.phymed.2015.10.001.







