Anesthesia for Patients Who Are Breastfeeding
Breast milk confers both direct and indirect infant benefits through at least 6 months of age and is recommended by the WHO and AAP to continue until 24 months. General anesthesia and most perioperative medications are compatible with breastfeeding. Physical separation from the infant may require a mother to pump, but discarding the expressed milk is rarely necessary.
Mothers of normal term or older infants can resume pumping or direct breast feeding without interruption following anesthesia as soon as they are awake and alert. This is consistent with recent guidelines by the American Society of Anesthesiologists and the Academy of Breastfeeding Medicine.
Preoperative
- Patients may continue to take clear liquids by mouth until 2 hours prior to their procedure to maintain adequate hydration.
- In addition to standard preoperative history and physical, interview the patient regarding the age and health of the infant. Preterm infants or those with chronic disease or apnea may be more sensitive to even trace amounts of sedative medication. In this rare case, a period of 4-6 hours pumping and discarding milk is typically adequate and involving the infant pediatrician may be helpful.
- Ask patient to breastfeed or pump in preoperative area, as close to the time of surgery as possible.
- Educate the patient and family that medications move into and back out of the milk. Current recommendations are that breastfeeding immediately after anesthesia is safe. They should monitor the baby for any signs of sedation or abnormal reactions.
- Regional blocks that would be expected to affect nipple sensation (anterior branch of lateral cutaneous nerve of the fourth thoracic nerve) may interfere with nipple stimulation, the let-down reflex, and the expression of milk for the duration of the block. This should be incorporated into the risk/benefit discussion with the patient and short duration, unilateral block, etc. should be considered.
Intraoperative
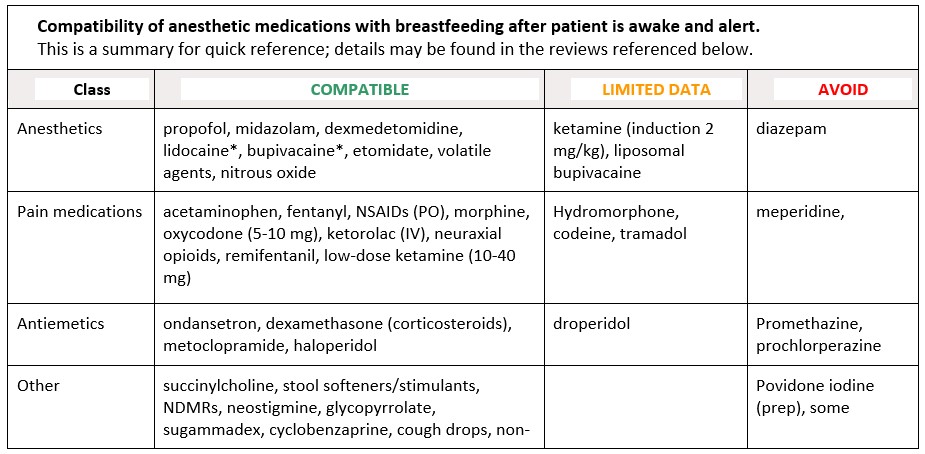
- Commonly used anesthetic medications are shown in the table below. Consider regional techniques and multimodal approach to pain management with non-opioid medications as primary therapy with opioids reserved for breakthrough. (Note that this is true of most patients, not specific to lactating patients.)
- Remifentanil and remimazolam are excellent choices for breastfeeding patients. These drugs are ultra-short acting, allowing for short recovery periods and therefore less exposure to the breastfed infant. They have predicable esterase metabolism, also present in infants, which further minimizes infant risk.
- Conscious sedation is also compatible with uninterrupted lactation once the patient is awake and alert when compatible medications are selected (see Table).
- Be aware of medications and dyes administered by the surgical team, most of which are compatible.
Compatibility of anesthetic medications with breastfeeding after patient is awake and alert.
This is a summary for quick reference; details may be found in the reviews referenced below.
Postoperative
- Encourage resumption of hydration and normal nutrition as early as possible.
- Postanesthetic shivering: As meperidine is not compatible with lactation (and tramadol is not preferred), we recommend non-pharmacologic management followed by low-dose dexmedetomidine
- Patients should use non-pharmacologic interventions and scheduled non-opioid medications as first-line for pain to limit potentially sedating medications if required for breakthrough.
- Regardless of opioid medication used, the lowest effective dose and shortest duration of therapy should be prescribed.
Even with careful planning, a lactating patient may experience a decrease in supply and may consider some supply recovery techniques or working with a lactation professional in the recovery period.
Written by Sarah Dodd, M.D., updated with support from Kaytlin Krutsch, PhD, PharmD
© S Dodd 2024
Sarah E. Dodd, M.D.
Kaytlin Krutsch, PhD, PharmD, MBA, BCPS
