Antibodies are a known benefit of breastfeeding. A specific type of antibody found in breastmilk, IgA, protects infants from infections. When breast milk coats the baby’s oral mucosa, nasal cavity, Eustachian tubes, and GI tract, the IgA binds to bacteria and viruses at that surface preventing them from entering the baby’s system. The foreign invader stays immobile in the GI tract and is digested and excreted instead of causing sickness. IgA is not found in infant formulas, and is personalized to the environment the mom (and baby) is exposed to.
Adaptive Immune System
Our immune system is complex and works in many capacities. Natural antibodies are proteins that are the backbone of the immune system. It responds to viruses, bacteria, fungi, and parasites (also called pathogens) that you come across every day. They are produced specifically to recognize and attack antigens (parts of the foreign pathogen(s)) currently present in your environment. Later, some antibodies can remember the antigen and facilitate a quicker immune response the next time you are exposed to that pathogen.
Antibodies & Breast Milk
Substances transfer into the breastmilk through the blood—if a substance isn’t present in the blood’s serum, chances are great that it will not be in the milk in relevant degrees. Some antibodies are produced by plasma cells to freely circulate in the bloodstream, allowing for the possibility of transfer into breastmilk. These free antibodies include IgG, IgM, and IgA, and are a large part of humoral immunity, linking the innate and adaptive immune systems through the activation of the complement system. For the topic of breastfeeding, cell-mediated immunity is less important as its major components are intracellular.
Not All Antibodies are the Same
Your body is constantly producing new antibodies that fight new pathogens that are present in your environment. During infection, the first antibodies produced are IgM antibodies and are transiently found in the blood and lymph. Both IgM, and later IgG, initiate pathways that mount a systemic response throughout your body. The systemic response is characterized by fever, elevated white blood counts, etc. Both IgG and IgM antibodies play similar roles in destroying harmful substances that enter our bodies. IgM is the fastest antibody produced, but it is short lived. IgG antibodies are overall the most common antibody and are found in all body fluids. IgG plays an important role in fighting bacterial and viral infections, and are the only type of antibody that can cross the placenta of a pregnant woman in order to help protect the fetus.
IgA is secreted into the blood, GI tract, and mucous membranes of moms and babies.1 Most antibodies are too large to transfer into breastmilk in large amounts. However, IgA is transported across the lactocyte barrier into the milk. IgA plays a very different role than IgG and IgM, which explains its added benefit for breastfeeding (more to come).
Antibodies & Infants
Following delivery, the infant will start producing their own antibodies as they are exposed to pathogens. Conversely, the levels of maternal IgG in the infant begin to fall shortly after delivery. This “inherited” protection will deteriorate over the first six months of life (Figure 1).2 Maternal IgA consumed from a breastfeeding infant can help protect an infant through this transition as they build their own immune defenses. Because the pathogens each person encounters are unique, each person’s antibodies are different than each other. A mother and her child are often in the same environments, and therefore exposed to the same pathogens. This is a huge benefit for antibodies in breastmilk—they are customized to protect the baby against the specific pathogens they are most likely to be exposed to.
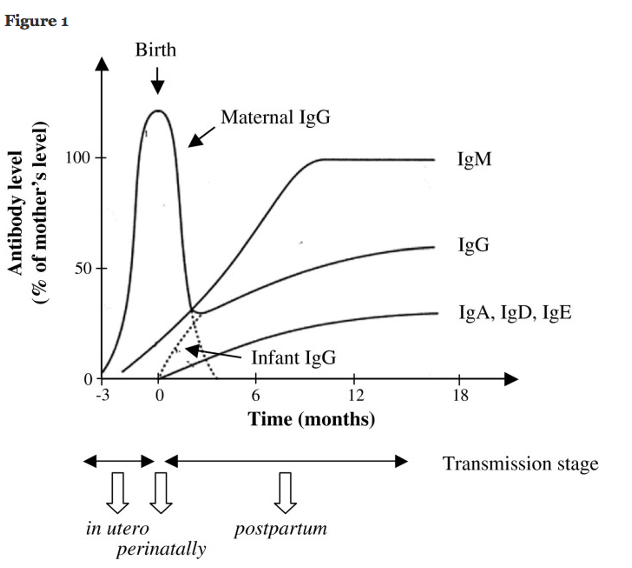
Figure 1: Infant Antibody Levels Over the First 18 Months of Life2
How SIgA Works
IgA is stabilized with a secretory component when it is transported across mucous membranes, becoming SIgA. The overall job of specific secretory immunoglobulin A (SIgA), is to inhibit initial pathogen colonization by performing immune exclusion both on the mucosal surface and within virus-infected secretory epithelial cells, all without causing tissue damage3. In short, SIgA antibodies function by binding to pathogens that come in contact throughout GI tract, effectively neutralizing them. Binding these foreign substances prevents them from entering the body. In essence, you can think of SIgA antibodies as our “first line of defense.”
As an infant breastfeeds, SIgA enters the infant’s GI tract (mouth, esophagus, stomach) via breast milk and coats the GI tract. Occasionally, breast milk can reach throughout the oropharynx, nasopharynx, and eustachian tubes (small tubes that run between the middle ear and upper throat). While this could be concerning for other liquids, breastmilk is transporting neutralizing SIgA antibodies anywhere it travels.
Additionally, it is thought that SIgA antibodies are highly resistant to digestion by enzymes that are located in the GI tract, such as pepsin which is known to be the key digestive enzyme located in the stomach. These antibodies are unlikely to be damaged via proteolysis due to the stabilizing secretory component.4
Will my child receive these antibodies via consumption of breast milk?
It depends on the type.
- Maternal IgG antibodies are delivered to the fetus while in utero via the placenta
- Maternal SIgA are present in breastmilk in large quantities (0.5-1.0 grams per day!)5
- Other maternal antibodies may be present in breastmilk. How much and how useful they are is up for debate.
Breast Fed Vs. Formula Fed?
The presence of maternal antibodies is the biggest difference (that we know of) between formula and breastmilk. With infants that are breast-fed, SIgA is known to be found in infant feces only two days after delivery and onset of breast-feeding. In contrast, infants that are formula fed, SIgA is not found in their feces until around one month postpartum once the infant is able to synthesize their own IgA antibodies (SIgA is not found in formula).4
Jordan Burkham, MSII
Kaytlin Krutsch, PharmD, MBA, BCPS
1. Hoffman W, Lakkis FG, Chalasani G. B Cells, Antibodies, and More. Clin J Am Soc Nephrol. Jan 7 2016;11(1):137-54. doi:10.2215/CJN.09430915
2. Braibant M, Barin F. The role of neutralizing antibodies in prevention of HIV-1 infection: what can we learn from the mother-to-child transmission context? Retrovirology. Oct 7 2013;10:103. doi:10.1186/1742-4690-10-103
3. Brandtzaeg P. Role of secretory antibodies in the defence against infections. Int J Med Microbiol. Apr 2003;293(1):3-15. doi:10.1078/1438-4221-00241
4. Andreas NJ, Kampmann B, Mehring Le-Doare K. Human breast milk: A review on its composition and bioactivity. Early Hum Dev. Nov 2015;91(11):629-35. doi:10.1016/j.earlhumdev.2015.08.013
5. Le Doare K, Kampmann B. Breast milk and Group B streptococcal infection: vector of transmission or vehicle for protection? Vaccine. May 30 2014;32(26):3128-32. doi:10.1016/j.vaccine.2014.04.020







