August 10, 2022
Summary:
Monkeypox is a viral infection that requires special consideration during pregnancy and breastfeeding: it is expected to transfer into breastmilk, and fetal infections have been reported (vertical transmission). The InfantRisk Center will discuss Monkeypox in these special populations, which vaccines are preferred, and an evaluation of the risks and benefits of treatment.
In this article:
Pregnancy, Breastfeeding, and Monkeypox
Pregnancy, Breastfeeding, and Monkeypox Vaccines
Pregnancy, Breastfeeding, and Monkeypox Treatments
What is Monkeypox?
Human monkeypox is a virus (Orthopoxvirus) with a presentation similar to smallpox. Clinical differentiation of the disease from smallpox or varicella is quite difficult. The monkeypox rash can also look similar to herpes simplex, varicella-zoster, or secondary syphilis infections. Human monkeypox was not recognized as a distinct infection until 1970, when the virus was isolated from a patient with suspected smallpox infection. Vaccination for smallpox prevents infections of monkeypox, but with the diminished use of smallpox vaccines, infections with monkeypox have arisen. Monkeypox can actually infect a large number of mammals, including squirrels and numerous other rodents. Although the virus is named monkeypox, monkeys are not the virus's origin.
How does Monkeypox spread?
Monkeypox spreads through person-to-person contact, including touch, body fluids, and inhalation from coughing, talking, or kissing. It is unknown if monkeypox transfers via semen or vaginal fluids, but it most certainly does from close contact. In the current outbreak, close contact with infectious skin lesions is the primary risk factor for acquiring the infection. Most of the clinical characteristics of human monkeypox infection mirror those of smallpox, although smallpox infections are more severe.
What are the symptoms of Monkeypox?
Symptoms often arise within 5 to 21 days after exposure to the virus, but most humans have symptoms by days 7 to 14. Initial symptoms include headache, fever, muscle aches, swollen lymph glands in the neck, and exhaustion. Enlarged lymph nodes are firm, tender, and sometimes painful.
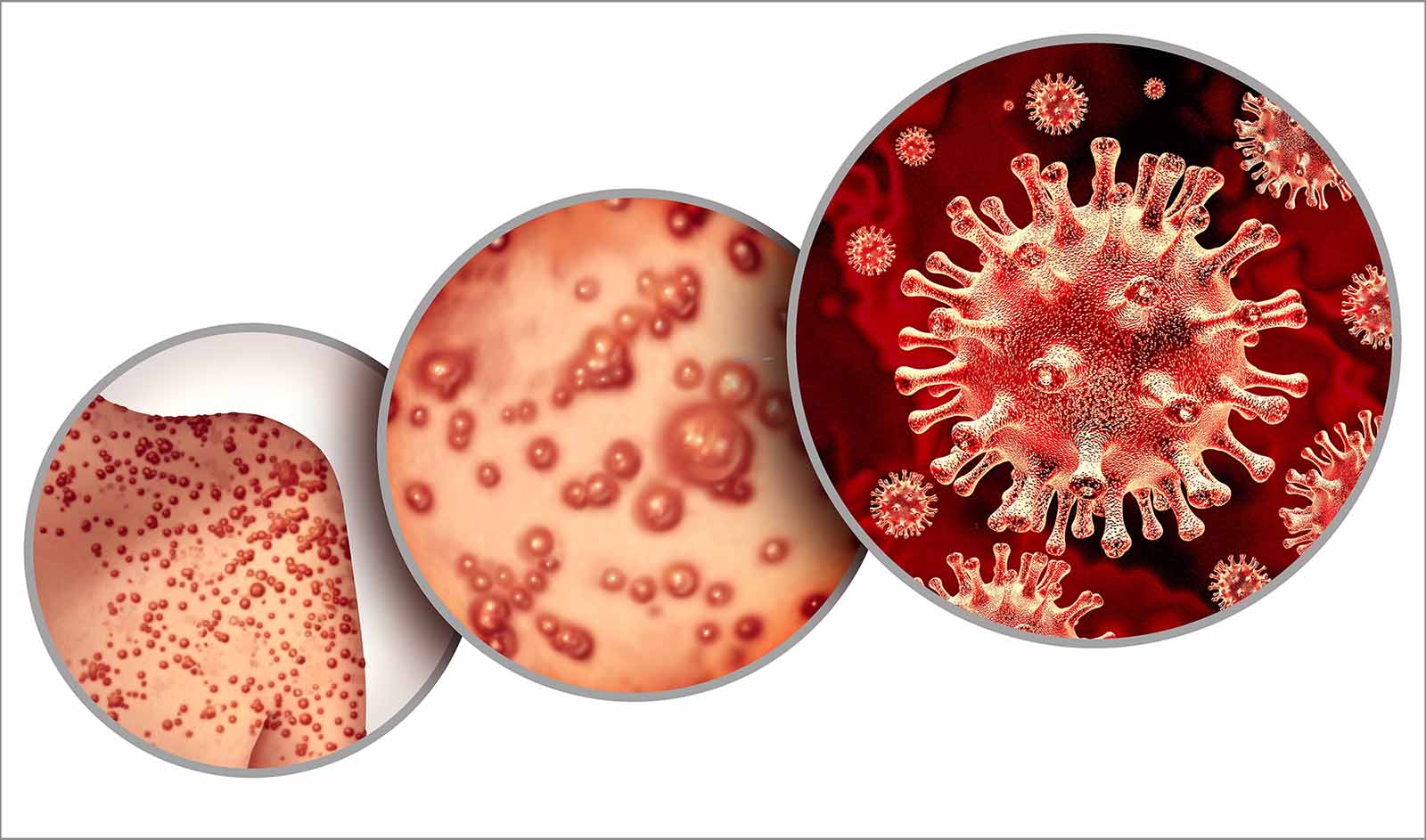
Within a few days, a skin rash develops, followed by eruptions of skin bumps that are painful and very itchy. These pustular bumps eventually scab over and drop off within 2 to 4 weeks. Lesions are often in the mouth and can cause difficulties with drinking and eating.
![]()
Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of High-Consequence Pathogens and Pathology (DHCPP)[KK1]
How dangerous is Monkeypox?
Monkeypox is usually a self-limiting illness, with symptoms lasting 2 to 4 weeks. However, some patients could experience serious illness. Hospitalization for monkeypox is very uncommon but may be necessary in those requiring care for nausea, vomiting, and swallowing issues that result in dehydration. Fatality rates in Africa have been reported as high as 10% in the 2022 outbreak, but deaths in the US and in other outbreaks have been rare. Details are still emerging.
Can you cure monkeypox?
While there is no cure for monkeypox, some antiviral medications may help prevent the worsening of symptoms and are discussed below. With or without the use of medications, an infant should not breastfeed during the recovery period.
What do we know about Monkeypox and Pregnancy?
There are several reported cases of virus transmission in utero at or before delivery. It is not yet known if monkeypox can increase the risk of miscarriage in pregnant women. However, historical evidence suggests an increased risk of miscarriage with smallpox and other viruses. Rare cases of stillbirth and preterm births have been reported.
It is unknown if monkeypox increases the risk of congenital disabilities, although high fevers which occur during the infection might lead to birth defects. There is simply no data presently on this risk.
Can you breastfeed with active Monkeypox or while you are being treated for this virus?
Currently, the CDC strongly recommends against breastfeeding with monkeypox. It is believed that the monkeypox virus will transfer into human milk, and more importantly, close contact can transmit the disease to the infant.
If the mother recovers and the lesions are healed (scabbed over and covered by normal skin), the infant could return to breastfeeding. However, it can easily take 4 weeks to reach this phase.
Can you get the vaccine while pregnant or breastfeeding?
Yes, pregnant and/or breastfeeding mothers can get Jynneos if the vaccine is necessary due to viral exposure to monkeypox. Another vaccine option, ACAM2000, is contraindicated (not recommended) while pregnant and is not ideal for breastfeeding.
Jynneos is a live, but non-replicating viral vaccine FDA-approved for preventing monkeypox infection. Thus, it will impart immunity but will not "grow and replicate" or cause monkeypox syndrome. In most cases, if you are at risk of contracting the disease, the risk of the vaccine is significantly less than that of the infection for you and your infant. Before receiving the vaccine while breastfeeding, consult with a physician concerning your infant's health and ability to withstand exposure to this vaccine. The FDA recommends using an intradermal dose rather than the approved subcutaneous dose for pregnant and breastfeeding women. Jynneos is also known as the modified vaccinia Ankara vaccine (MVA), Imvanex (in the EU), and Imvamune (in Canada).
ACAM2000 is an FDA-approved vaccination against smallpox, made available by the FDA through expanded access for monkeypox. It is a live vaccine that is still capable of replicating and has more adverse effects. Jynneos is the preferred choice for at-risk pregnant or breastfeeding mothers. However, if Jynneos is unavailable, talk to your physician about the risks of being vaccinated with ACAM2000 compared to the risk of monkeypox infection.
ACAM2000 will produce a localized infection at the injection site (called a "take"). The lesion starts as a sore that then blisters, scabs, and heals to leave a scar over several weeks. The vaccination site should be covered to avoid transferring the live virus to other people. Direct contact with the site via sharing towels, swimming, etc., should be avoided until the site is completely healed, particularly with immunocompromised people.
While no human data is available for these specific vaccines during pregnancy or breastfeeding, the InfantRisk Center recommendations are based on decades of experience with other live and live-attenuated vaccines. Presently, only people with viral exposure are recommended to get the vaccines. This implies that their risk of viral infection would likely outweigh the risks of vaccination.
According to the CDC, "Benefits of vaccinating pregnant women usually outweigh potential risks when the likelihood of disease exposure is high, when infection would pose a risk to the mother or fetus, and when the vaccine is unlikely to cause harm." CDC. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR 2011; 60 (No. 2): 26.
Treatments for Monkeypox:
Treatment is usually limited to symptomatic care and the prevention of viral spread with isolation, hand washing, and face masks until lesions are healed. Symptomatic care includes pain management for the lesions. As more severe illness is usually due to dehydration, ensure adequate fluid intake.
Pregnant or breastfeeding people may be considered at risk for severe disease, which could qualify them for antiviral therapy.
Antiviral: Tecovirimat (TPOXX or ST-246)
The CDC recommends tecovirimat as first-line therapy for the treatment of active monkeypox for pregnant, recently pregnant, or breastfeeding people. Tecovirimat (TPOXX or ST-246) is an antiviral medication FDA-approved for treatment of smallpox in adults and children. Tecovirimat is expected to have antiviral activity against the monkeypox virus and is authorized for this indication by the FDA under an expanded access protocol.
Pregnancy: No human data is available for the use of tecovirimat in pregnant women or their infants. In animal studies (mice, rabbits), no embryofetal developmental toxicities were observed at maternal tecovirimat exposures up to 23 to 24 times human exposure at the recommended dose. It is not known if treatment with tecovirimat during pregnancy prevents congenital monkeypox.
Lactation: There is no human or animal data on tecovirimat and lactation. Tecovirimat will likely transfer into breastmilk, but only to a low level. Considering the lack of severe adverse effects, full breastfeeding may be reasonable for most mothers if both mom and infant are infected with monkeypox. Uninfected infants should not breastfeed from a mother with confirmed monkeypox virus, even during treatment. The most common infant adverse effects are expected to be vomiting and diarrhea. Mothers or babies that have impaired liver function should be more cautious, including an in-depth conversation of the risks versus benefits of your individual situation.
Antiviral: Cidofovir and Brincidofovir (CMX-001)
Cidofovir and brincidofovir have been considered alternative antiviral therapies to treat monkeypox infection. They are incorporated into viral DNA, slowing viral replication of the orthopoxvirus over time. Brincidofovir is a modified version of cidofovir that is converted to cidofovir within the cell. Cidofovir and brincidofovir are not recommended during pregnancy or breastfeeding. There are no human studies and limited animal studies on these drugs, but the small molecules are likely to result in significant fetal-infant drug exposure.
In animal studies, cidofovir produced external, soft tissue, and skeletal abnormalities in rabbit offspring at very low doses. As such, these medications should not be used to treat the monkeypox virus during the first trimester of pregnancy.
In adults, adverse effects of cidofovir include immunosuppression, reduced kidney function, and decreased intraocular pressure (vision changes). Brincidofovir has less nephrotoxicity than cidofovir; it displays different, but similarly concerning adverse effects such as changes in liver function and swelling.
Treatment for Severe Disease: Vaccinia Immune Globulin Intravenous (VIG-IV)
VIG-IV is pooled, purified human IgG (and trace IgA) derived from healthy plasma donors who previously received smallpox vaccines. There are no animal or human studies on vaccinia immune globulin intravenous (VIG-IV) during pregnancy or lactation. However, immune globulins have been widely used during pregnancy for many years without any apparent negative reproductive effects. An individualized risk-benefit analysis should take place between patient and provider for shared-decision making in these situations. IgG is generally poorly transferred into human milk; the IgG in VIG-IV is unlikely to cause risk in a breastfed infant. Endogenous secretory IgA is found in copious amounts in human milk but is produced at the lactocyte rather than transferred across the membrane. It is unlikely that IgA found in VIG-IV would transfer into milk in significant amounts.